





Insulin Pump for Diabetes: Endocrinologist view!


Table of Contents
- What is an insulin pump?
- Let’s talk about Sam.
- How does an insulin pump work?
- The pump also does insulin delivery with great precision
- There are many kinds of insulin pumps
- What type of insulin is used in an insulin pump?
- Will I still need to check my blood sugar every day?
- An insulin pump is a small device
- Who might use an insulin pump?
- What are the downsides of an insulin pump?
- How do people wear or carry their pump in real life?
- How do I decide if I should switch to an insulin pump?
- How to maintain and troubleshoot an insulin pump:
- In summary
What is an insulin pump?
Continuous subcutaneous insulin, or the insulin pump, has gained popularity and sophistication in recent years. An insulin pump is a device that delivers insulin to the body. Some people with diabetes use an insulin pump instead of shots to get their insulin treatment.
So why is an insulin pump different, and can it make a difference in your diabetes control? What is an insulin pump anyways? And no, it does not look like a morphine pump or breast pump. Let's have a look.
Let’s talk about Sam.
Sam is a type 2 diabetic. He has had diabetes for years. He is already on insulin multiple times daily. Sam understands that diabetes is a progressive disease. Insulin was not a punishment or the end of the road. It was just a milestone. From now on he knows he has to deal with insulin.
He is wondering what the best way is to take insulin. He feels that injecting insulin 4 times a day can be a burden. But he also knows the consequences of not taking insulin. He wants to have a long healthy life. He has a sense of responsibility. One day his endocrinologist talks to him about insulin pumps. He's heard about them before.
He has seen a few people using insulin pumps, too. Yet, he has heard mixed things about insulin pumps. Some people love it and some hate the insulin pump. He wonders why there are so many different opinions about insulin pumps. He starts by asking the question, how an insulin pump works. Let's answer his question.
How does an insulin pump work?
An insulin pump attaches to the body and delivers insulin under the skin. Pumps release insulin at a steady rate for basal insulin. Basal insulin is the insulin that the body needs to keep blood sugar at a normal rate. It is like the amount of gas your car burns in order to run at neutral/idle speed.

Pumps also give a bolus of insulin following data entered by the patient for carbohydrates consumed in meals. Think like your car needing more gas when you push on gas when you gain speed from neutral/idle speed. This is called bolus insulin. The pump does all that without an insulin needle injection since it is already connected to you via the skin.
Insulin adjustments are is easier with the insulin pump.
The pump also does insulin delivery with great precision
People with an insulin pump have more choices about when and what they eat. They don't always have to plan their meals in advance. That is because the insulin pump uses computer calculations. Pumps, for example, can give Sam 1.2 units of basal insulin between midnight and 3 am.
Starting at 3 am the pump can increase hourly basal insulin delivery from 1.2 units/hour to 1.4 units while Sam is sleeping and so on. This is possible because Sam’s doctor can program the pump based on Sam’s personal needs. Sam’s doctor knows that Sam’s blood sugar significantly starts rising after 4 am.
So, he makes a change in basal insulin rate to make sure Sam wakes up to his day with a good blood glucose. Similarly, Sam’s insulin pump for diabetes can also calculate the insulin he needs for mealtimes (bolus insulin) based on the pre-programmed rate.
Sam still must enter how much carbs he is eating into the pump. Sometimes a small percentage of people cannot learn carb counting easily for a variety of reasons. Those people can also manually enter bolus insulin manually per their doctor's instruction. Now Sam is more curious about insulin pumps. He asks about the types of insulin pumps. He heard there are different brands out there and wants to find out which approach will be best for him.
There are many kinds of insulin pumps
Some insulin pumps are connected to a tube that you insert under your skin, usually in the belly area. But other body areas can also be used. This involves using a small auto inserter tiny needle (or a device that has a small needle). After insertion, the needle comes out and small tiny catheter stays under the skin. Think like a miniature form of an IV line but it's under the skin with a push of a button on the inserter.
It should not hurt more than a single needle injection. The good part is that you will not have to put any needle on your skin for the next 2-3 days. The pump itself, the part that holds insulin and small computer part can be attached to your clothing or carried in your pocket. Insulin Pumps in this category are Medtronic insulin pump and Tandem.
Another type of pump sticks directly to the skin. You use a syringe to fill it with insulin. This pump called Omnipod (In one of the blog articles we compare pumps. Please refer to that article later to know more about individual brands).
Then, when you press a button, the device inserts a tiny tube into your skin to deliver the insulin. The pump is covered with a patch and left in place for 2 to 3 days. After this, the pump needs to be replaced with a new one in a different area of the body.
What type of insulin is used in an insulin pump?
Only short-acting (regular) or rapid-acting insulins are used with an insulin pump for diabetes. Most people use rapid-acting insulin with a pump. This could be Humalog, NovoLog, Apidra, Novolin R, or Humulin R . If you use a pump, your doctor or nurse will help you figure out the amount of insulin that you should get.
Will I still need to check my blood sugar every day?
Just like people who use insulin shots, people with an insulin pump need to check their blood sugar level a few times each day. On the other hand, if you are using Dexcom G6 or Freestyle Libre you may not have to check your blood sugar at all. Or, you may need to check your blood sugar only occasionally. Some insulin pumps have connections with continuous glucose monitoring system such as Dexcom G6 and Freestyle Libre. For example, tandem pumps work with Dexcom G6. This is called the Control IQ system.
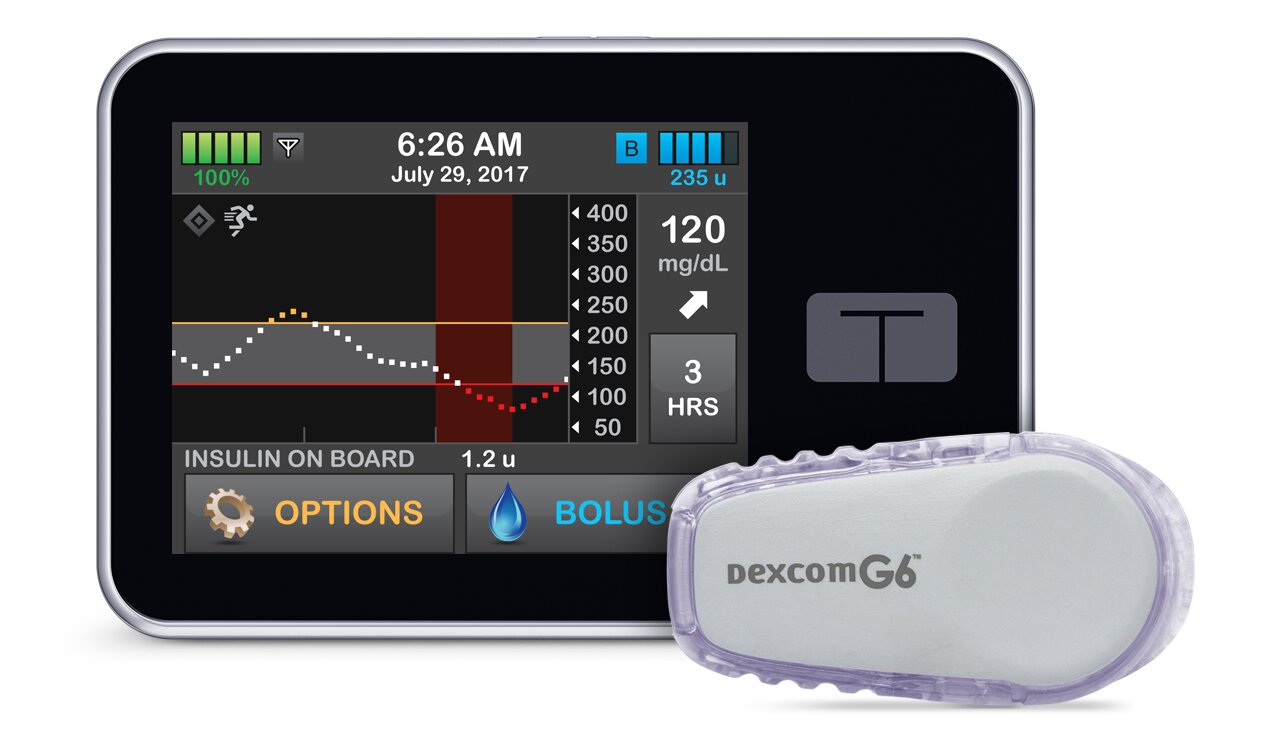
With the Control IQ system, the insulin pump can adjust insulin delivery for basal and bolus insulin. It does not totally replace the patient's involvement in bolus insulin delivery. On the other hand, it can compensate for the small mistakes a patient can make due to the miscalculation of carbohydrates or the effect of stress and exercise.
Medtronic systems use their own sensors. Those CGMs are called Guardian. Guardian CGM systems can be more sensitive for picking up low or high blood sugars. On the other hand, they are known to have many false-positive results which can be frustrating.
The bottom line, using an insulin pump might help people keep their blood sugar levels under better control, with fewer episodes of low blood sugar. This can even be more enhanced with the use of a continuous glucose monitoring system such as Dexcom G6, freestyle libre or Medtronic guardian.
For a more thorough review of different types of pumps please refer to our previous blog post about which insulin pump to choose. Sam is concerned about carrying a device on his body. He asks his endocrinologist his opinion about the inconvenience associated with caring an insulin pump on his body all the time.
An insulin pump is a small device
Most insulin problems are the size of an old school pager. New age iPods may look similar to the available insulin pumps. Most of the time they are half the size of a cell phone. They can be carried just like a small cell phone or a pager. Most people who are on insulin but not on insulin pumps must carry their insulin pens. They also must carry pen needles and make calculations for their insulin.
In addition, they need to attach the needle to the pen. Finally, they need to expose their skin to give the injection, etc. All of these inconveniences make an insulin pump an attractive option for people who have a busy lifestyle or for people who do not want to deal with multiple steps for giving an insulin injection especially when they are outside. So yes, if you get an insulin pump for diabetes, you will need to wear or carry it on your body all the time.
Who might use an insulin pump?
People of all ages can use an insulin pump for their diabetes management. Most often, insulin pumps are used in people with type 1 diabetes. Patients with type 2 diabetes who need multiple daily injections of insulin are also a candidate for the insulin pump. People who suffer from fluctuating blood sugars will benefit from insulin pumps. People who have a lot of low blood sugars will also benefit from insulin pumps.
Remember a diabetic insulin pump is computerized insulin delivery. It makes it a lot easier to control insulin delivery. This helps avoid significant fluctuations and prevent low blood sugars (hypoglycemia). There will be a modest improvement in A1c as well. If you refer to our A1c blog, A1c itself does not really tell much about blood sugar fluctuations or low blood sugars.
That is important to understand. Someone with a blood sugar of 6.5% may have more blood sugar fluctuations than someone with an A1c of 9%. Until this point, Sam seems to be very convinced that an insulin pump can help him. On the other hand, he also now needs to know the downsides of insulin pumps.
What are the downsides of an insulin pump?
The downsides of an insulin pump include the following:
- It may take time to learn how to program and use an insulin pump.
This is honestly more of a problem for older patients or patients who are not highly motivated.
- If the tube comes out of the skin or gets a kink, Sam won't get any insulin.
Then their blood sugar level can get too high, which can lead to serious problems. On the other hand, if Sam understood that he will need to keep an eye on his blood sugars either via fingersticks or via CGM he would identify the problem on time. This will help fix it before it becomes a bigger problem.
During his training, Sam also learned that if he thinks that there is a problem with the insulin pump he needs to use back up. So, if blood sugars are not improving after bolus via an insulin pump, he will need to use his regular insulin pen to correct his blood sugars. Thankfully, this problem does not happen too often with insulin pumps. There are also ways to prevent kinks if they happen too frequently.
- Insulin pumps usually cost more than insulin shots.
This is a general statement. As long as pump supplies do not cost too much most patients end up saving money on insulin. This is because they end up using only one type of insulin. So for example, if someone is using a Lantus, Tresiba or Toujeo for basal insulin and NovoLog for bolus before the pump, he will end up using only NovoLog for his insulin pump and stop using Lantus.
- Wearing or carrying an insulin pump all the time can be bothersome.
As we discussed before, carrying an insulin pump can be an inconvenience. Yet, carrying an insulin pen, pen needles and supplies can also be an inconvenience. Not to mention, with an insulin pen you will still have to expose your skin and give an injection every time. You will also have to do calculations yourself. Or, you will have to plan for your meals every time.
- The area where the tube goes into the skin can get infected. On the other hand, if Sam follows simple hygienic instructions this should not be a big problem at all.
How do people wear or carry their pump in real life?
People with diabetes wear or carry their insulin pumps in different ways. They can put it in their waistband, shorts, underwear, or bra. They can also keep it in their pocket or clip it to a belt. At night, people with diabetes can put their insulin pump in their pajamas or clip it to a blanket, sheet, or pillow.
Most people can disconnect their pump and take it off for short periods of time, about 1 to 2 hours. That way, people don't need to wear it when they shower, bathe, swim, or have sex.
How do I decide if I should switch to an insulin pump?
After reading this blog article you must have a good idea. Moreover, you, your doctor, and your family will need to discuss whether an insulin pump is right for you. To help you decide, discuss the benefits and downsides of using a pump and your individual situation.
How to maintain and troubleshoot an insulin pump:
- Change the needle and tubing every 2 to 3 days. You need to refill your insulin pump with insulin every few days.
- Change the battery on schedule
- Make sure the date and time are correct on your insulin pump.
- Keep an eye on the pump body and case for any cracks. Call the insulin pump company to get replacements if you note any structural problem. Your pump may lose water resistance with cracks.
- Check the tubing for air bubbles occasionally and when you replace it.
- Monitor your insertion site for infection or bleeding.
- Discuss with your diabetes specialist and diabetes coach to make sure that rates and ratios used for the pump are accurate.
- If you are changing insulin pumps or upgrading pumps for diabetes make sure your endocrinologist knows about it and makes the transition.
- Always have backup basal and bolus insulin in case the pump fails.
- Try to have an online account. Most diabetic insulin pump companies provide free accounts. Free accounts help you keep a record of your past settings in case of insulin pump failure. It also helps your endocrinologist to monitor you remotely if needed.
- As a diabetic patient make sure you have glucagon injection handy. Also, let your family members know who to call for your diabetes-related matters when you are not able to.
- If your blood glucose reading is abnormally high, take a corrective dose of insulin, and test again in one to two hours. If your blood sugars are remaining high or going higher check for ketones. Do a correction fast-acting insulin to bring the blood sugar down while you also change out the tubing, reservoir, and infusion set. Keep a close watch to see if this works.
- If you are using a continuous glucose monitoring system such as Dexcom G6 pay attention to alerts. Make sure you set up at the alerts correctly. Freestyle libre does not really have alerts. When your blood sugars are too high or too low from any CGM system double-check with a glucose fingerstick.
In summary
At www.sugarmds.com we are dedicated to helping you choose the best way to manage your diabetes. Insulin pumps are another tool to help achieve diabetes goals. You do not have to have an insulin pump to be a successful diabetic on insulin. It is very important to discuss that with your endocrinologist and diabetes coach. Do not worry about contacting us or give us a call.
We will evaluate your unique, individual situation. This will not be a one-time deal. Our patients stay in touch with us 24/7. They can ask their questions anytime, anywhere. We do not limit them to a 15 to 30-minute consultation to get all their questions out. Anytime you have trouble with an insulin pump or CGM system, you know you have someone you can trust and reach out regardless of time and date or location.
Written By Dr. Ahmet Ergin
463 total articles
Meet Dr. Ahmet Ergin, a highly skilled and dedicated endocrinologist with a passion for diabetes care. Dr. Ergin earned his medical degree with honors from Marmara University in Istanbul. He completed internal medicine residency and endocrinology fellowship at Cleveland Clinic. Dr. Ergin is board-certified in Internal Medicine, Endocrinology, Diabetes, and Metabolism due to his vast medical expertise. He's a certified diabetes educator, author of “The Ultimate Diabetes Book,” and founder of “the SugarMD YouTube channel.” Dr. Ergin offers exceptional diabetes care to his patients in Port Saint Lucie, FL, helping them manage effectively. For a closer look into his insights and experiences, connect with Dr. Ahmet Ergin on LinkedIn, Instagram, and YouTube.”
Disclaimer: These statements have not been evaluated by the Food and Drug Administration. Information on this website isn't intended to treat, cure or prevent any disease. Discuss with your doctor and do not self-treat.
Products











