
UP TO 40% OFF SITEWIDE






Types of Foot Ulcers: Understanding Common Types


Table of Contents
- Importance of Understanding Foot Ulcers
- Early Detection and Treatment
- Prevention of Serious Complications
- Connection to Other Health Conditions
- Improving Quality of Life
- Incorporating Supplements for Support
- Educating the Public and Healthcare Providers
- Economic Impact
- Types of Foot Ulcers
- Ischemic Ulcers
- Diabetic Foot Ulcer
- 5 Ways to Prevent Diabetic Ulcers
- 1. Regular Foot Inspections
- 2. Proper Footwear
- 3. Control Blood Sugar Levels
- 4. Avoid Smoking
- 5. Seek Professional Care
- Venous Stasis Ulcers
- Arterial Ulcers
- Symptoms and Causes of Foot Ulcers
- Blood Vessels and Poor Circulation
- Pressure Points and Varicose Veins
- Treatment and Prevention
- Healing Wounds and Preventing Infection
- Foot and Ankle Care
- Conclusion
- About The Author
Foot ulcers are a prevalent and often overlooked medical condition that can significantly impact a person's quality of life. These open sores, found on the foot's surface can vary in severity and type. They may appear on the bottom of the feet the tips of the toes or anywhere in between. Understanding the types of foot ulcers, including the main keyword "types of foot ulcers," is not merely a matter of medical curiosity but a vital aspect of healthcare that affects millions of people worldwide.
The complexity of foot ulcers lies in their multifaceted nature. They are not merely a symptom but often a sign of underlying health issues. From poor circulation and high blood pressure to more specific conditions like diabetes, foot ulcers can be both a cause and a consequence of serious health problems.
Importance of Understanding Foot Ulcers
Early Detection and Treatment
Foot ulcers can be deceptive. What might appear as a minor sore can quickly escalate into a severe ulcer if left untreated. Early detection and understanding of the types of foot ulcers can lead to timely treatment, reducing the risk of complications. This includes recognizing common types such as ischemic ulcers, venous stasis ulcers and diabetic foot ulcers.
Prevention of Serious Complications
Untreated foot ulcers can lead to infections that may spread to other parts of the body.
In extreme cases, this can result in the need for amputation. Understanding the signs and symptoms of foot ulcers, including the role of poor blood flow and varicose veins can prevent such dire outcomes.
Connection to Other Health Conditions
Foot ulcers are often linked to other health conditions such as diabetes and high blood pressure.
Recognizing a foot ulcer can be a critical step in diagnosing these underlying issues. For instance, a diabetic foot ulcer may be the first sign of uncontrolled blood sugar levels.
Improving Quality of Life
Chronic foot ulcers can lead to ongoing pain and discomfort, limiting mobility and independence. By understanding how to prevent and treat these ulcers, individuals can maintain an active lifestyle.
This includes awareness of pressure points, proper foot and ankle care and the importance of blood vessels in maintaining foot health.
Incorporating Supplements for Support
Products like SugarMD Neuropathy Support can play a role in protecting nerves from damage caused by conditions that lead to foot ulcers. Understanding how supplements can complement traditional treatments adds another layer of care and prevention.
Educating the Public and Healthcare Providers
Knowledge about foot ulcers should not be confined to medical professionals.
Public awareness campaigns and education can empower individuals to take control of their foot health. This includes understanding the risks associated with poor circulation the bottom of the feet's vulnerability and the importance of regular check-ups.
Economic Impact
The cost of treating foot ulcers can be substantial, especially if complications arise. Preventive measures, early detection and appropriate treatment can reduce healthcare costs and the economic burden on individuals and the healthcare system.
Types of Foot Ulcers
Foot ulcers are a prevalent and often severe health concern that can lead to significant discomfort and complications if not properly addressed. Among the various types of foot ulcers, ischemic ulcers and diabetic foot ulcers are particularly common and noteworthy. Understanding these specific types is essential for recognizing their unique characteristics and underlying causes.
Ischemic Ulcers
Ischemic ulcers, also known as arterial ulcers, are a type of foot ulcer that occurs when there is a lack of blood flow to a particular area of the foot. This lack of blood flow is often caused by peripheral arterial disease (PAD), where the arteries become narrowed or blocked.
Characteristics
Ischemic ulcers typically appear on the tips of the toes, foot or heel. They are often characterized by a pale or bluish color, with well-defined edges. The surrounding skin may be cool to the touch and the affected area may be painful, especially during walking.
Causes
The primary cause of ischemic ulcers is poor blood flow, often resulting from conditions that affect the arteries. These can include:
- Atherosclerosis: This condition involves the hardening and narrowing of the arteries, reducing blood flow to the extremities.
- High Blood Pressure: Chronic high blood pressure can damage the arteries, leading to reduced blood flow.
- Smoking: Smoking can contribute to arterial diseases by causing constriction and damage to the blood vessels.
Understanding the underlying causes of ischemic ulcers is crucial for early detection and proper care as these ulcers can lead to serious complications if left untreated.
Diabetic Foot Ulcer
Diabetic foot ulcers are a specific type of foot ulcer that occurs in individuals with diabetes. These ulcers are particularly concerning due to the high prevalence of diabetes worldwide and the potential for severe complications.
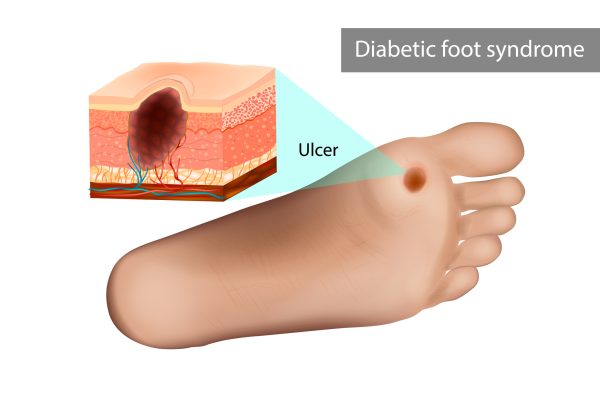
Characteristics
Diabetic foot ulcers often appear on the bottom of the feet, where pressure and friction are most common. They may vary in appearance, ranging from shallow red craters to deep wounds that can expose underlying tissues. The surrounding skin may be callused or discolored.
Causes
The development of diabetic foot ulcers is often multifactorial, with several underlying causes contributing to their occurrence:
- Neuropathy: Diabetes can lead to nerve damage, known as neuropathy which reduces sensation in the feet. This lack of sensation can make it difficult to detect minor injuries or pressure points, leading to the development of ulcers.
- Poor Circulation: Diabetes can also affect blood flow, leading to poor circulation in the extremities. This reduced blood flow can slow the healing process, making the foot more susceptible to ulcers.
- Foot Deformities: Individuals with diabetes may develop foot deformities that increase pressure on specific areas of the foot, contributing to ulcer formation.
Diabetic foot ulcers are a significant concern as they can lead to infections and other serious complications. Early detection and understanding of these ulcers are vital for effective care and prevention.
5 Ways to Prevent Diabetic Ulcers
Diabetic foot ulcers are a significant concern for individuals with diabetes. These ulcers can lead to severe complications if not treated properly. Here are five effective ways to prevent diabetic ulcers:
1. Regular Foot Inspections
Daily foot inspections are crucial for anyone with diabetes. Look for any signs of redness, swelling, cuts or pressure points. Early detection of these signs can prevent the development of ulcers. Using a mirror can help inspect hard-to-see areas and if you notice anything unusual, consult a healthcare provider immediately.
2. Proper Footwear
Wearing the right shoes is vital in preventing diabetic foot ulcers. Shoes should fit well without being too tight or too loose. They should provide adequate support and cushioning, especially at the bottom of the feet and the tips of the toes. Custom-made diabetic shoes are available that take into consideration the unique shape and pressure points of an individual's feet.
3. Control Blood Sugar Levels
High blood sugar levels can cause damage to blood vessels and nerves, leading to poor circulation and sensation in the feet. Regular monitoring and control of blood sugar levels are essential in preventing these complications. A balanced diet, regular exercise and proper medication can help maintain optimal blood sugar levels.
4. Avoid Smoking
Smoking can reduce blood flow to the extremities, including the feet. Reduced blood flow can lead to poor healing of wounds and increase the risk of ulcers. Quitting smoking is a crucial step in preventing diabetic foot ulcers.
5. Seek Professional Care
Regular check-ups with healthcare providers specializing in foot care are essential. Podiatrists can assess the condition of the feet, provide necessary treatments and offer guidance on proper foot care practices. Regular professional care can detect potential problems early and prevent the development of ulcers.
By following these five preventive measures, individuals with diabetes can significantly reduce the risk of developing foot ulcers. It requires consistent care, awareness and collaboration with healthcare providers.
Venous Stasis Ulcers
Venous stasis ulcers, also known as venous leg ulcers, are a type of wound that occurs when the venous valves fail to function properly. These valves are responsible for returning blood from the legs to the heart. When they become damaged or weakened, blood can pool in the legs, leading to increased pressure in the veins.
This pressure can cause the skin to break down and form an ulcer. The development of venous stasis ulcers is often associated with varicose veins, a condition where the veins become enlarged and twisted. Varicose veins are more than just a cosmetic concern; they can lead to serious health problems, including venous stasis ulcers. Venous stasis ulcers typically appear on the inner part of the leg, just above the ankle.
They may start as a discolored area and gradually develop into an open sore. The surrounding skin may become hardened or thickened and the ulcer itself may produce a foul-smelling discharge. Several factors can contribute to the development of venous stasis ulcers, including obesity, lack of physical activity and a history of deep vein thrombosis (DVT). Age is also a significant risk factor as the valves in the veins can weaken over time.
Understanding the underlying causes of venous stasis ulcers is essential for proper care and management. While this section does not cover treatment or prevention, it's worth noting that addressing the root causes can be a crucial step in healing and preventing these ulcers.
Arterial Ulcers
Arterial ulcers, on the other hand, are caused by a lack of blood flow to the affected area. Unlike venous stasis ulcers which are related to the return of blood to the heart, arterial ulcers are associated with the delivery of blood to the extremities. Arterial ulcers are often a sign of peripheral arterial disease (PAD), a condition where the arteries become narrowed or blocked.
This can reduce blood flow to the limbs, leading to the formation of ulcers. The lack of oxygen and nutrients can cause the skin and underlying tissues to break down, forming an open sore. These ulcers are typically found on the outer part of the leg the foot or the tips of the toes. They can be extremely painful, especially at night or when the legs are elevated.
The skin surrounding an arterial ulcer may appear pale or shiny and the ulcer itself may have a "punched-out" appearance. Risk factors for arterial ulcers include smoking, diabetes, high blood pressure and high cholesterol.
These factors can lead to atherosclerosis, a condition where fatty deposits build up in the arteries, restricting blood flow. Arterial ulcers can be a serious health concern as they may indicate an underlying cardiovascular issue. Proper diagnosis and understanding of the specific type of ulcer are vital for appropriate care.
Symptoms and Causes of Foot Ulcers
Foot ulcers are complex conditions that can arise from various underlying issues. Understanding the symptoms and causes is essential for early detection, proper diagnosis and effective treatment. This section will delve into the critical aspects of blood vessels, poor circulation, pressure points and varicose veins, all of which play a significant role in the development of foot ulcers.
Blood Vessels and Poor Circulation
Poor circulation and blood vessel issues are at the core of many foot ulcers. Let's explore these aspects in detail:
Poor Blood Flow: Reduced blood flow to the feet can lead to ischemic ulcers. Conditions like peripheral artery disease (PAD) and high blood pressure can cause poor circulation, depriving the tissues of essential oxygen and nutrients.
This deprivation can lead to the formation of ulcers, particularly on the tips of the toes and the bottom of the feet.
Diabetes and Blood Vessels: Diabetes can damage blood vessels, leading to poor blood flow. This damage often results in diabetic foot ulcers which are common and can be challenging to heal.
Arterial Ulcers: Arterial ulcers are caused by a lack of blood flow to the affected area. These ulcers are often painful and can appear on the foot where blood flow is most restricted.
Symptoms of Poor Circulation: Symptoms may include cold feet, numbness, tingling and pain. The skin may appear pale or bluish and wounds may heal slowly or not at all.
Pressure Points and Varicose Veins
Pressure points and varicose veins are other significant factors contributing to foot ulcers. Here's how they play a role:
Pressure Points: Pressure points on the foot, often caused by ill-fitting shoes or prolonged standing can lead to the development of ulcers. These pressure sores can break down the skin, leading to open wounds that are susceptible to infection.
Varicose Veins: Varicose veins are enlarged, twisted veins that can cause venous stasis ulcers. These ulcers usually occur on the lower legs and are caused by malfunctioning valves in the veins, leading to blood pooling and increased pressure.
High Blood Pressure and Varicose Veins: High blood pressure can exacerbate varicose veins, leading to further complications and the development of ulcers.
Symptoms of Pressure Points and Varicose Veins: Symptoms may include swelling, pain, discoloration and hardened skin around the affected area.
Treatment and Prevention
Understanding the treatment and prevention of foot ulcers is vital for maintaining overall foot health. The process involves a combination of medical intervention, self-care and lifestyle changes. Let's delve into the essential aspects of healing wounds and caring for the foot and ankle.
Healing Wounds and Preventing Infection
Healing wounds and preventing infection is a multifaceted approach that requires both professional medical care and diligent self-care.
- Wound Cleaning: Regular cleaning of the wound with a gentle cleanser helps in removing debris and bacteria. It's essential to keep the wound moist to promote healing.
- Medication Application: Depending on the type of ulcer, specific medications such as antibiotics or topical creams may be prescribed to aid in healing and prevent infection.
- Dressing Changes: Proper dressing of the wound with sterile bandages helps in protecting the wound from external contaminants. Changing dressings regularly as directed by a healthcare provider is crucial.
- Off-loading Pressure: Utilizing special footwear or devices to redistribute pressure away from the ulcer can accelerate healing. This is especially important for ulcers caused by pressure points.
- Monitoring for Signs of Infection: Keeping an eye out for signs of infection, such as increased redness, swelling or foul odor, is vital. Early detection and treatment of infection can prevent complications.
- Lifestyle Changes: Healthy eating, controlling blood sugar levels (for diabetic ulcers) and avoiding smoking can significantly impact the healing process.
- Professional Care: Regular visits to healthcare providers for wound assessment and care are essential. They can adjust treatment plans as needed and ensure that the wound is healing properly.
Foot and Ankle Care
Proper foot and ankle care is not only essential for treating ulcers but also for preventing them. Here's how to take care of your feet:
- Regular Inspections: Daily examination of the feet for any signs of redness, swelling or sores can lead to early detection and treatment.
- Proper Footwear: Wearing shoes that fit well and provide adequate support can prevent pressure on sensitive areas.
- Foot Hygiene: Keeping the feet clean and dry helps in preventing fungal infections and other complications.
- Moisturizing: Regular moisturizing of the feet helps in preventing dryness and cracking which can lead to ulcers.
- Avoiding Prolonged Pressure: Shifting weight and avoiding standing for extended periods can prevent pressure ulcers.
- Professional Foot Care: Regular visits to a podiatrist or foot care specialist can help in maintaining foot health and addressing any concerns early.
Conclusion
Foot ulcers are a serious health concern that can lead to significant discomfort and complications if not treated properly. Understanding the types of foot ulcers, recognizing the symptoms and taking proactive steps in treatment and prevention can make a substantial difference in foot health. Healing wounds, preventing infection and proper foot and ankle care are integral to this process.
By embracing a comprehensive approach that combines medical intervention with self-care and lifestyle changes, one can effectively manage and prevent foot ulcers. Whether dealing with ischemic ulcers, diabetic foot ulcers or other types the key lies in early detection, proper care and a commitment to overall foot health.
About The Author
Meet Dr. Ahmet Ergin a highly skilled and dedicated endocrinologist with a passion for diabetes care. Dr. Ergin earned his medical degree with honors from Marmara University in Istanbul. He completed internal medicine residency and endocrinology fellowship at Cleveland Clinic.
Dr. Ergin is board-certified in Internal Medicine, Endocrinology, Diabetes and Metabolism due to his vast medical expertise. He's a certified diabetes educator, author of "The Ultimate Diabetes Book," and founder of "the SugarMD YouTube channel."
Dr. Ergin offers exceptional diabetes care to his patients in Port Saint Lucie, FL, helping them manage effectively. Disclaimer: These statements have not been evaluated by the Food and Drug Administration. Information on this website isn’t intended to treat, cure or prevent any disease. Discuss with your doctor and do not self-treat.
Written By Dr. Ahmet Ergin
466 total articles
Meet Dr. Ahmet Ergin, a highly skilled and dedicated endocrinologist with a passion for diabetes care. Dr. Ergin earned his medical degree with honors from Marmara University in Istanbul. He completed internal medicine residency and endocrinology fellowship at Cleveland Clinic. Dr. Ergin is board-certified in Internal Medicine, Endocrinology, Diabetes, and Metabolism due to his vast medical expertise. He's a certified diabetes educator, author of “The Ultimate Diabetes Book,” and founder of “the SugarMD YouTube channel.” Dr. Ergin offers exceptional diabetes care to his patients in Port Saint Lucie, FL, helping them manage effectively. For a closer look into his insights and experiences, connect with Dr. Ahmet Ergin on LinkedIn, Instagram, and YouTube.”
Disclaimer: These statements have not been evaluated by the Food and Drug Administration. Information on this website isn't intended to treat, cure or prevent any disease. Discuss with your doctor and do not self-treat.
Products



