
UP TO 40% OFF SITEWIDE





VITAMIN D DEFICIENCY: HOW IT CAUSES DIABETES


Table of Contents
- What Is Vitamin D?
- What Happens If You Are Vitamin D Deficient?
- How Do You Get Vitamin D?
- Symptoms of Vitamin D3 Deficiency
- How is This Vitamin Related to Diabetes?
- Can Vitamin D2 or D3 Supplement Fix Insulin Resistance?
- How Does Vitamin D Supplementation Lower Insulin Resistance?
- What is my verdict about Vitamin D?
- About the author:
At the moment, vitamin D deficiency seems to be common and is linked to the cause of many diseases, such as metabolic problems, including insulin resistance and diabetes.
What Is Vitamin D?
Vitamin D is a fat-soluble vitamin that helps your body do a lot of essential things, like keep your bones, teeth, and joints healthy and help your immune system work.
What Happens If You Are Vitamin D Deficient?
Vitamin D is essential for good health, but many people don't get enough of it. This is especially true for overweight individuals and those who are insulin resistant. Vitamin D deficiency can lead to inflammation and cell damage, making it more difficult for the body to regulate blood sugar levels and store fat. As a result, obese and insulin-resistant individuals are more likely to suffer from vitamin D deficiency.
Additionally, vitamin D deficiency has been linked to an increased risk of type 2 diabetes, further complicating the relationship between obesity, insulin resistance, and vitamin D levels. While getting more vitamin D is vital for everyone, it is especially crucial for those struggling with their weight or blood sugar levels.
How Do You Get Vitamin D?
Vitamin D has long been known as the "sunshine vitamin" because our bodies produce it in response to exposure to sunlight. In recent years, however, researchers have discovered that vitamin D has a number of other health benefits. It helps to build strong bones, prevents certain types of cancer, and boosts the immune system. Now, it appears that vitamin D may also help to prevent insulin resistance and diabetes.
A new study has found that vitamin D deficiency is one of the factors that can accelerate the formation of insulin resistance. Vitamin D helps to prevent epigenetic alterations associated with insulin resistance and diabetes. So we can say that vitamin D deficiency is one of the factors that can accelerate the formation of insulin resistance.
Symptoms of Vitamin D3 Deficiency

Signs and symptoms of Vitamin D deficiency.
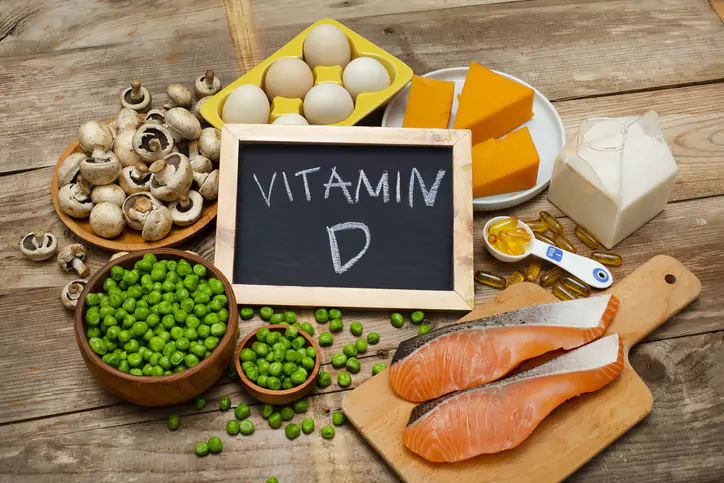
Vitamin D3 is an essential vitamin that helps the body absorb calcium and phosphorus. It is found in food sources such as fatty fish, eggs, and fortified milk, and it can also be produced by the body when skin is exposed to sunlight. However, vitamin D3 deficiency is relatively common, especially in people who have dark skin or who do not get enough sun exposure.
Symptoms of vitamin D3 deficiency can include bone pain and weakness, muscle cramps, and fatigue. In severe cases, vitamin D3 deficiency can lead to Rickets, a condition that causes softening and deformities of the bones. If you think you may have a vitamin D3 deficiency, it is important to see a doctor for a blood test. Treatment typically involves taking a supplement or increasing your exposure to sunlight.
Recently, the vitamin D receptor (VDR) and vitamin D-metabolizing enzymes were discovered in various types of cells, such as pancreatic -cells and insulin-responsive cells like adipocytes. These findings are significant because they show that vitamin D is metabolized in multiple types of cells. Adipose tissue is not only a major source of adipokines and cytokines, both essential components of the systemic inflammatory response. It is also where a significant amount of vitamin D is stored.
There is evidence that vitamin D seems to control a number of events that take place in order to let the pancreatic -cells make insulin and control the level of glucose in the blood. Both vitamin D2 (also known as ergocalciferol) and vitamin D3 fall under the category of the vitamin D moniker (cholecalciferol). Vitamin D can be obtained by people in a number of ways, including exposure to sunlight, consumption of particular foods, and the use of nutritional supplements like SugarMD Neuropathy Suppport and SugarMD Diavitamin!
How is This Vitamin Related to Diabetes?
Insulin resistance leads to the development of diabetes. Insulin resistance causes beta cells that make insulin die off, leading to high blood sugar, or diabetes. Pre-clinical studies have shown that vitamin D can control how much insulin is made and how long pancreatic cells live. Several studies have shown that vitamin D deficiency makes it harder for pancreatic -cells to release insulin in response to glucose.
It also appears that taking vitamin D may make it possible to restore the way glucose makes insulin release when needed. Some clinical studies found that vitamin D supplements can improve insulin secretion. Vitamin D is important not only for the function of -cells in the pancreas but also for insulin-sensitive tissues like fat, liver, and skeletal muscle. Many studies have shown that vitamin D makes the body more sensitive to insulin.
Can Vitamin D2 or D3 Supplement Fix Insulin Resistance?
Having said that "If you're a typical, overweight, or obese middle-aged man or woman, taking a vitamin D pill probably won't make a big difference in your chance of getting type 2 diabetes. But it might have an effect if you take it along with a healthy diet and exercise or if your diet is naturally high in vitamin D and you also live a healthy lifestyle. Researchers watched 2,423 people for 2.5 years.
Half took 100 micrograms (mcg) of vitamin D daily, while the other half didn't take any supplements. At the end of the trial, the New England Journal of Medicine published the results, which showed that people who took vitamin D supplements had more vitamin D in their blood. During the study, they were 12% less likely to get type 2 diabetes, but this was slightly different from the group that didn't get any supplements.
There have been a lot of lab studies that show that vitamin D is good for beta cells and that it is also good for reducing inflammation in general. And we know that type 2 diabetes is linked to metabolic syndrome, which is usually a state with a lot of inflammation. So vitamin D deficiency may lead to insulin resistance.
How Does Vitamin D Supplementation Lower Insulin Resistance?

Insulin Resistance
Vitamin D may also lower insulin resistance by affecting how calcium and phosphorus are used in the body and by making the insulin receptor gene work better. In a study with 5,677 people who had trouble handling glucose, adding vitamin D increased insulin sensitivity by 54%.
Another study of 126 healthy people showed that there is a direct link between insulin sensitivity and 25(OH)D level and that a lack of vitamin D made pancreatic -cells work less well. Vitamin D apparently raises the amount of calcium in the cells, making it easier for glucose to get into the muscles. Vitamin D.
PPAR also controls peroxisome proliferator-activated receptor (PPAR) in the nucleus is an important part of insulin sensitivity and is controlled by vitamin D. Increased inflammation is linked to not getting enough vitamin D. Vitamin D also lowers the expression of proinflammatory cytokines like interleukins, IL-1, IL-6, and TNF-a that are linked to insulin resistance. It also lowers the activity of NF-Kb (Nuclear factor).
What is my verdict about Vitamin D?
The following is how I see it. Vitamin D is not just a vitamin. It is actually a hormone that regulates many functions in the body, such as the function of beta cells, which is responsible for the production of insulin; the metabolism of calcium and bone, which is linked to insulin resistance; and an important regulator of inflammation and fat cells.
If you are overweight, you will have more fat stores, reducing vitamin D's effect on your body. Because of this, you will need to take more vitamin D in order to make up for that vitamin D deficiency. On the other hand, losing weight and allowing vitamin D to become unbound is the most effective solution to the issue. Keep in mind that vitamin D is a fat-soluble vitamin which is stored in your body's fat cells.
Extra fat will prevent vitamin D from being released from your cells and into the bloodstream. Therefore, you can free up your vitamin D stores by dieting, exercising, and fasting, as well as by taking vitamin D supplements and eating foods rich in vitamin D. Thank you for reading this article. If you found it useful please share with family and friends! And Remember a little vitamin D a day can save a doctor's visit.
About the author:

Who is Dr. Ergin?Dr. Ahmet Ergin is an endocrinologist interested in and passionate about diabetes care. Dr. Ergin earned his medical degree with honors at Marmara University School of Medicine in Istanbul, Turkey. Then, he completed his internal medicine residency and endocrinology fellowship at Cleveland Clinic in Cleveland, Ohio.
He is a board-certified Internal Medicine and Endocrinology, diabetes, and metabolism physician. He is also a certified diabetes education specialist.
Disclaimer: Any information on diseases and treatments that may be found on this website is provided solely for the purpose of providing general guidance and should never, under any circumstances, be used in place of the advice provided by your physician or another qualified healthcare professional. When you have questions or concerns about your current medical condition, you should never hesitate to consult with your primary care physician or another appropriately trained healthcare professional.
Written By Dr. Ahmet Ergin
465 total articles
Meet Dr. Ahmet Ergin, a highly skilled and dedicated endocrinologist with a passion for diabetes care. Dr. Ergin earned his medical degree with honors from Marmara University in Istanbul. He completed internal medicine residency and endocrinology fellowship at Cleveland Clinic. Dr. Ergin is board-certified in Internal Medicine, Endocrinology, Diabetes, and Metabolism due to his vast medical expertise. He's a certified diabetes educator, author of “The Ultimate Diabetes Book,” and founder of “the SugarMD YouTube channel.” Dr. Ergin offers exceptional diabetes care to his patients in Port Saint Lucie, FL, helping them manage effectively. For a closer look into his insights and experiences, connect with Dr. Ahmet Ergin on LinkedIn, Instagram, and YouTube.”
Disclaimer: These statements have not been evaluated by the Food and Drug Administration. Information on this website isn't intended to treat, cure or prevent any disease. Discuss with your doctor and do not self-treat.
Products













