UP TO 40% OFF SITEWIDE






Side effects of Glipizide, Glimepiride or Glyburide


Table of Contents
- What are Glipizide, Glimepiride, or Glyburide(Sulfonylureas) & What are the Main side effects?
- Why do sulfonylureas have such a bad reputation?
- How does Glipizide, Glimepiride, and Glyburide( Sulfonylureas) work?
- Mechanism of action of sulfonylureas.
- Why the main side effects of sulfonylureas (glipizide, glimepiride, glyburide) can be weight gain and low blood sugars?
- Is Kidney Failure a Problem or Increase the Risk of Side Effects of Glipizide, Glyburide, and Glimepiride?
- What are the alternative medications for sulfonylureas (glipizide, glyburide, glimepiride) with Fewer Side Effects?
What are Glipizide, Glimepiride, or Glyburide(Sulfonylureas) & What are the Main side effects?
One of the most commonly prescribed medications is sulfonylureas (glipizide, glimepiride, glyburide). They are generally taken once or twice a day 30 minutes before a meal. You can take sulfonylureas on your own or alongside other diabetes drugs such as metformin.
They work by stimulating your pancreas to make insulin in a non-glucose-dependent manner. Due to continuous insulin production main side effects of glipizide, glimepiride, or glyburide( Sulfonylureas) are low blood sugar and weight gain.
There are many other long-term side effects of glipizide, glimepiride, or glyburide (sulfonylureas) which is the main topic of this article. Unfortunately, sulfonylureas are not necessarily the best medications. They have been in the market for a long time.
Side effects and problems associated with sulfonylureas have become more and more clear over time. The most common side effects of glipizide, glimepiride, or glyburide( Sulfonylureas) are weight gain and hypoglycemia (low blood sugar), beta-cell failure, and possible heart-related complications.
Why do sulfonylureas have such a bad reputation?
In addition to the weight gain and low blood sugar side effects, there is some scientific evidence out there that makes them less popular. Here are a few examples:

How beta cells respond to glipizide, glyburide, glimepiride
1. Beta cells are the main insulin-producing cells in the pancreas. There are scientific suggestions that sulfonylureas may accelerate pancreatic beta-cell failure. This was demonstrated by their lack of durability in maintaining blood sugar control in the UK Prospective Diabetes Study (UKPDS) and ADOPT (A Diabetes Outcome Progression Trial) study.
The same issue was raised by Ralph de Fronzo in his 2008 American Diabetes Association’s Banting lecture, in which he noted that: ‘Sulfonylureas are not recommended because, after an initial improvement in glucose control, they are associated with a progressive rise in HbA1c and progressive loss of beta-cell function.
Pancreatic beta-cell apoptosis( cell death) is key in the progression of diabetes and poor long-term diabetes outcomes. As the pancreas loses the ability to secrete insulin due to beta-cell exhaustion, patients end up needing insulin earlier rather than later.
As we discussed, sulfonylureas act upon these beta cells, and constant stimulation of beta cells to work without rest may accelerate this “burn-out” process. This mechanism is one of the main side effects of sulfonylureas (glipizide, glimepiride, glyburide) we approach sulfonylureas with caution. Within 1 to 2 years, sulfonylureas begin to lose their effectiveness in some patients.
Heart-related implications about glipizide, glyburide, glimepiride.
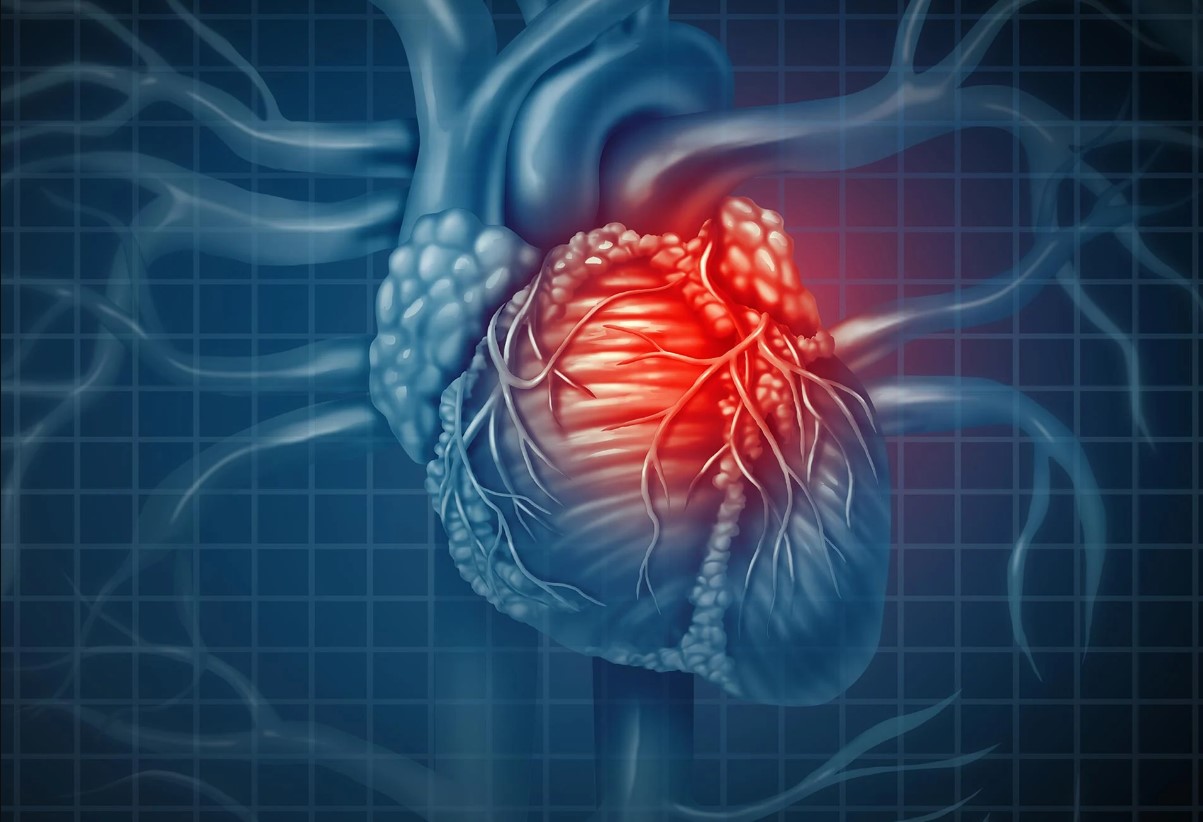
2. Some studies suggest that treatment with sulfonylureas may be associated with side effects and poorer outcomes in patients who have a heart attack as well. Especially some studies indicate glyburide may possibly worsen the outcome after a heart attack. The majority of studies with no major designed-related biases reported increased risks of cardiovascular events and mortality with sulfonylureas.
How does Glipizide, Glimepiride, and Glyburide( Sulfonylureas) work?
Mechanism of action of sulfonylureas.
Sulfonylureas (glipizide, glimepiride, glyburide) and meglitinides (repaglinide, nateglinide) directly stimulate insulin release from the pancreas and reduce blood glucose concentrations. Because they work by stimulating insulin secretion, they are useful only in patients with remaining pancreatic function.
Why the main side effects of sulfonylureas (glipizide, glimepiride, glyburide) can be weight gain and low blood sugars?
Since insulin production becomes continuous and not based on the needs of the patient after using sulfonylurea medication, the patient has to eat in order to prevent low blood sugar. As a result, one of the main side effects of glipizide, glimepiride, or, glyburide (sulfonylureas) is low blood sugar below 70 mg/dl.
This is counterintuitive for diabetes management. We ask patients to reduce the carbohydrates in their diet better and yet prescribe a medication that can increase the appetite and cause low blood sugars if patients try to diet.
Is Kidney Failure a Problem or Increase the Risk of Side Effects of Glipizide, Glyburide, and Glimepiride?

How do kidneys play a role in glipizide, glyburide, and glimepiride metabolism?
The kidney is the organ that metabolizes all of the sulfonylureas except repaglinide which is actually meglitinide( a different class that works similarly) not necessarily a sulfonylurea.
As a result, kidney dysfunction puts you at a significant risk of developing low blood sugars if you are on sulfonylureas which are another side effect of glipizide, glimepiride, or, glyburide (sulfonylureas).
If you are on glipizide, glimepiride, or, glyburide (sulfonylureas) you have to be careful about those situations in which hypoglycemia (low blood sugar) is most likely to occur.
They are as follows:
- After exercise or if you miss a meal.
- When the medication dose is too high (if you are having frequent low blood sugars you should reduce the dose of glipizide, glyburide, or glimepiride)
- With the use of longer-acting drugs (glyburide or extended-release formulations)-glyburide has the highest risk of low blood sugar among sulfonylureas.
- If you are undernourished or have alcohol intoxication.
- Should you have impaired kidney or heart function or gastrointestinal disease you also have to be careful using sulfonylureas
- With concurrent therapy with salicylates, sulfonamides, fabric acid derivatives (such as gemfibrozil), and warfarin as these agents can reduce the clearance of sulfonylureas (glipizide, glyburide, glimepiride)
- After being in the hospital medication needs may change after hospital admission.
- Are there any patient groups that can benefit from glipizide, glimepiride, or, glyburide (sulfonylureas) without side effects?
Patient groups that we use sulfonylurea successfully are MODY patients with mutations in the HNF1A( MODY 3) and HNF4A gene( MODY 1), two of the three most common MODY subtypes. In these patients, we use glipizide, glimepiride, or glyburide successfully.
The rest of the patients with type 2 diabetes are not great candidates for sulfonylureas due to their significant side effect profile such as frequency of low blood sugar and weight gain.
What are the alternative medications for sulfonylureas (glipizide, glyburide, glimepiride) with Fewer Side Effects?
Nowadays we have a lot of medications that do not cause weight gain and actually can lead to a lot of weight loss. Also, many diabetic medications do not have low blood sugar risks anymore either. Since we can choose medications that can lead to weight loss rather than weight gain, without the risk of low blood sugar we prefer using non-sulfonylurea agents when possible.
Sometimes if the patient cannot afford the higher quality medications we may have to use sulfonylureas. They still will bring blood sugar down with all the side effects of glipizide, glimepiride, or, glyburide (sulfonylureas).
Although sulfonylureas are not the best medications to use it is better to have a relatively controlled blood sugar than having totally uncontrolled blood sugar. We will just have to deal with the side effects of glipizide, glimepiride, or, glyburide (sulfonylureas) adjust our lifestyle more intensively, and monitor blood sugars more frequently.
GLP-1 classes such as Ozempic, rybelsus, Trulicity, and Victoza are great agents that are more effective than sulfonylureas. GLP-1 class medications also induce significant weight loss compared to weight gain with sulfonylureas.
These medications also do not cause low blood sugars unless you are also on insulin or sulfonylurea drugs. Most agents and GLP-1 classes such as Ozempic, Trulicity, and Victoza have proven to be beneficial for the heart and reduce the risk of heart attacks and strokes significantly.
On the other hand, there are a lot of studies suggesting that sulfonylureas may increase the risk of heart attacks and strokes. Also medications and GLP-1 class are very safe for kidney failure with the exception of exenatide (Bydureon, Byetta).
SGLT2 inhibitors such as Jardiance, Farxiga, Steglatro, and Invokana also have shown significant benefits in reducing the risk of heart attacks and heart failure and multiple studies. They also do not cause low blood sugars and they can induce significant weight loss.
They do not have side effects of glipizide, glimepiride, or, glyburide (sulfonylureas). Metformin and pioglitazone still remain popular although weight loss from metformin is very minimal and pioglitazone can lead to weight gain. Their advantage is their low cost as well as low risk of low blood sugar.
They also do not have side effects of glipizide, glimepiride, or, glyburide (sulfonylureas). Compared with metformin, sulfonylureas have shown 24% to 61% increased risk for death from all causes. Compared to metformin, some of the sulfonylureas have shown an 18% to 30% increased risk for heart failure.
Compared to metformin, treatment with Actos was linked to 31% to 39% decreased risk of death. I hope this article helped you understand the side effects of glipizide, glimepiride, or, glyburide (sulfonylureas) and understand your other options. Please continue to come back and visit our website for weekly articles.
Written By Dr. Ahmet Ergin
465 total articles
Meet Dr. Ahmet Ergin, a highly skilled and dedicated endocrinologist with a passion for diabetes care. Dr. Ergin earned his medical degree with honors from Marmara University in Istanbul. He completed internal medicine residency and endocrinology fellowship at Cleveland Clinic. Dr. Ergin is board-certified in Internal Medicine, Endocrinology, Diabetes, and Metabolism due to his vast medical expertise. He's a certified diabetes educator, author of “The Ultimate Diabetes Book,” and founder of “the SugarMD YouTube channel.” Dr. Ergin offers exceptional diabetes care to his patients in Port Saint Lucie, FL, helping them manage effectively. For a closer look into his insights and experiences, connect with Dr. Ahmet Ergin on LinkedIn, Instagram, and YouTube.”
Disclaimer: These statements have not been evaluated by the Food and Drug Administration. Information on this website isn't intended to treat, cure or prevent any disease. Discuss with your doctor and do not self-treat.
Products